In this article we examine the key elements necessary to determine if you are evaluating a solution that has merely added the platform buzzword to compensate for future ideas on the roadmap, or if the solution has an architecture designed to achieve agility, flexibility, and extensibility.
Let’s start with a perspective on technology design. Good user interface design is a harmony of form and function, orchestrating a user’s workflow toward a task to be done. Good system design is clean organization and abstract thinking applied to building robust small pieces, and then ensuring those pieces work cleanly together and in a repeatable way, like Lego blocks.
The lack of true platform design in healthcare solutions is an ever-present problem. As a technology leader inside of health systems, I work with clinical and operation leaders to identify problems and map them to solutions. This objective requires market analysis and ultimately a build-vs-buy decision, where most health systems lean toward buying solutions off the shelf, or minimizing a custom build.
Most solutions in the market are small, focused, and rigid, solving a piece of the overall equation, resulting in 60% coverage of the true end-to-end problem. Therefore, an addional solution would be needed to cover the rest, but it too would typically be slightly off the mark and cover 30%. To make the solution viable, the remaining 10% coverage would require custom glue and compromise.
This decision process creates slowness from multiple vendor contracts, different user interfaces, and a lack of data interoperability ultimately referred to as a fragmented solution. When the next problem to solve or new requirement comes along in the form of a new medical procedure, a different service line, an expansion of the IDN, a new regulation, or a national pandemic, the lack of extensibility of this pieced-together solution shows its rigidness and limitations, often referred to as a point solution.
How does a “true platform” address this issue? Let’s examine the key elements of a true platform that helps your organization achieve agility, flexibility, and extensibility.
First, investigate the sentiment in the brainstorming sessions to feel out if you are working with a true platform. The easy things should be easy, the hard things possible, and the future things experimentable without intense resources. Are you able to add workflows onto the platform in a cohesive way? As you expand usage, value and speed should be exponential, not declining or linear.
Let’s consider tangible characteristics to hone in on this evaluation.
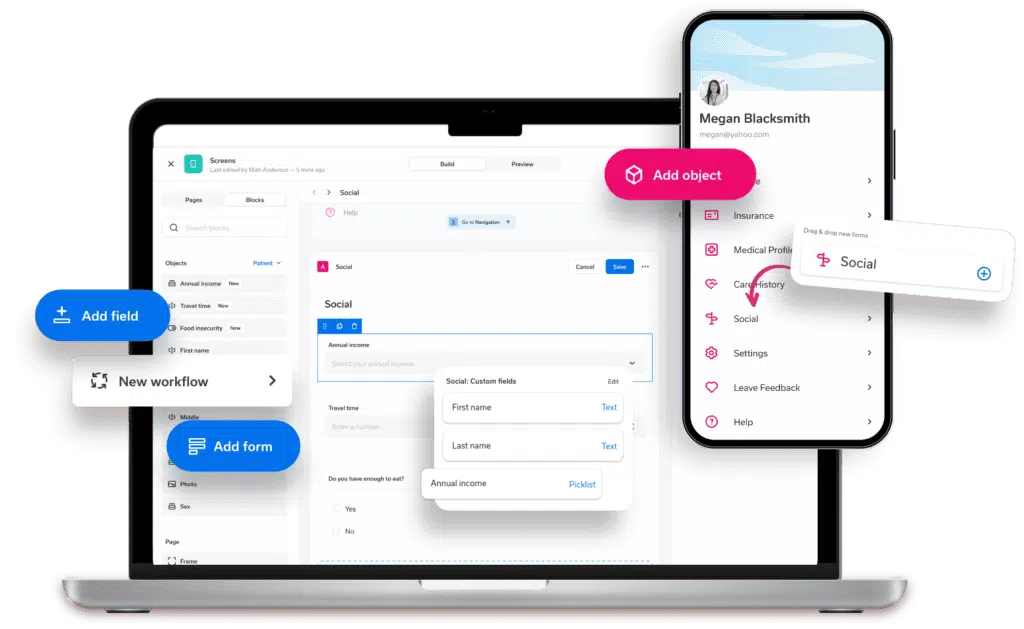
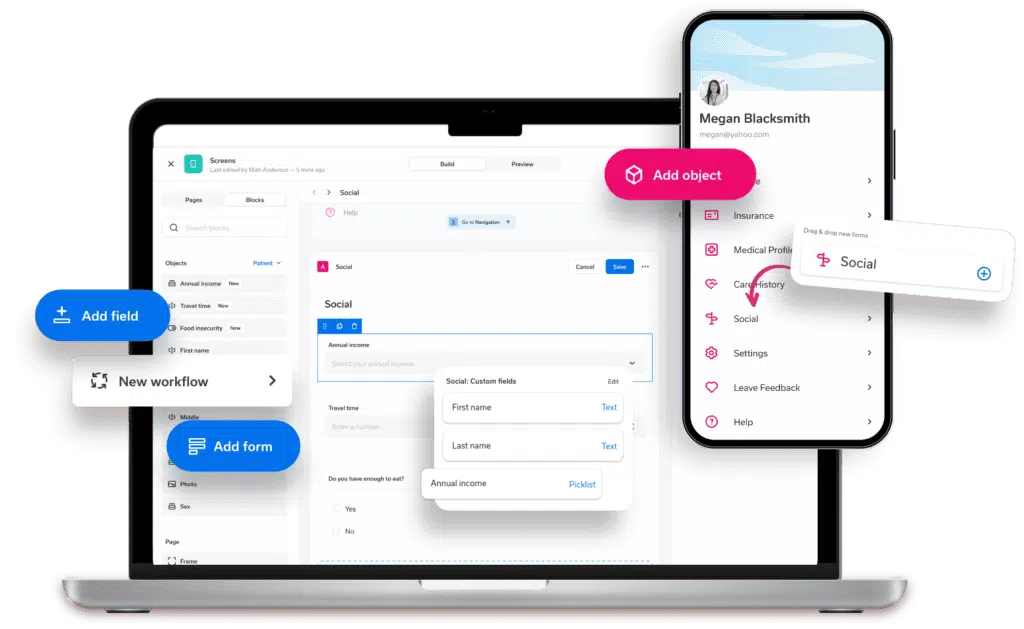
Configuration driven
Is the solution hard-coded or dynamic? Is it extensible to evolving requirements and new areas without complicating futue upgrades and enhancements? Engagements should be personalized for the health system and users, offering condition-specific experiences.- Data collection example Your primary care team wants to add depression screening questions to its new patient intake form. Can this task be done through a forms engine configuration—or is it a “feature on the roadmap”, or an addition that requires costly customization?
- Communication template example Your cardio team wants to add heart health education material to the end of appointment reminder emails. Can this task be done with a simple email update, or is the content hardwired into the template?
- Data insight-to-action example Your MSK/Ortho service line wants to better manage total joint replacement procedures by monitoring successful journeys in the candidate population. Can you create a specific dashboard that allows you to explore and engage appropriate patients, track the funnel of engagement and outcomes, and build reports regarding program performance?
Composable
Can system components be compiled easily to solve for varying workflows across different service lines?- Reuse example The pulmonary group focusing on high-risk COPD patients wants to design a remote monitoring protocol that couples patient care plans with a To-Do checklist to help them understand their medications. They will also be asked a few survey questions about nighttime breathing. Depending on the information captured, the team wants to automatically offer an appointment scheduling prompt to book a patient chronic care management visit. Can your administrators build this new workflow from existing components used elsewhere in the system?
Self service console
Does the system empower you to manage configurations and workflow builders that you can learn over time, or do all configurations need to be submitted as a ticket to the vendor, incurring extra costs?- Empowerment example New regulation requires the legal team to adjust language within several digital consent forms and add one additional question to the new patient check-in form. Can your team make these changes without requiring a larger solution engineering engagement?
- Agility example The population health team has seen some success in automated breast cancer screening outreach campaigns; they now want to slow mammography outreach and enable targeting for colonoscopies. Can the team pause, adjust, and resume campaigns with a command and control rules engine?
- Data sync example When trying to charge co-pays in the growing number of virtual visits, the front office revenue cycle team has been tracking a concerning trend regarding invalid insurance information. They need a solution that can read the latest insurance on file in the EMR, and prompt the user to validate or update the information during scheduling. If any of the information changes, the solution should pass the revised information back to both the EMR and a separate ambulatory billing system, which should ensure that the complexity of the various systems is masked and automated away for users.
Orchestration between modules
Solutions will often grow to have several modules, but does the left hand talk to the right hand in a cohesive way? A poorly merged acquisition could have taken place, or two teams may function without a unified company-wide strategy. Does 1+1=3 as you use more of the system? Value should be exponential, not linear.- Multi-site, multi-disciplinary complex workflow example The clinical quality team has been using the documentation improvement module to gain a better risk patient profile. They are understanding comorbidities and illness severity and want to leverage this information at discharge for high-touch care transitions and patients at risk for readmission. Can the solution take the derived data from CDI, dynamically update care plans, and trigger automated outreach follow-ups with open-ended questions to check in on a patient? The remote monitoring care navigators want to use the communications module to review and respond to the patient and ensure proper next steps are happening such as establishing a specialist appointment, adhering to their medication, and hooking up the blood pressure monitoring device.
- Omni-channel referral example The behavioral health team wants to convert more referrals from PCPs and patients leaving the ED. Can the solution personalize the outreach and offer SMS, email, app, or mobile web engagement channels? Can it generate referral recommendations that consider insurance, distance, sub-speciality mapping, and physician availability?
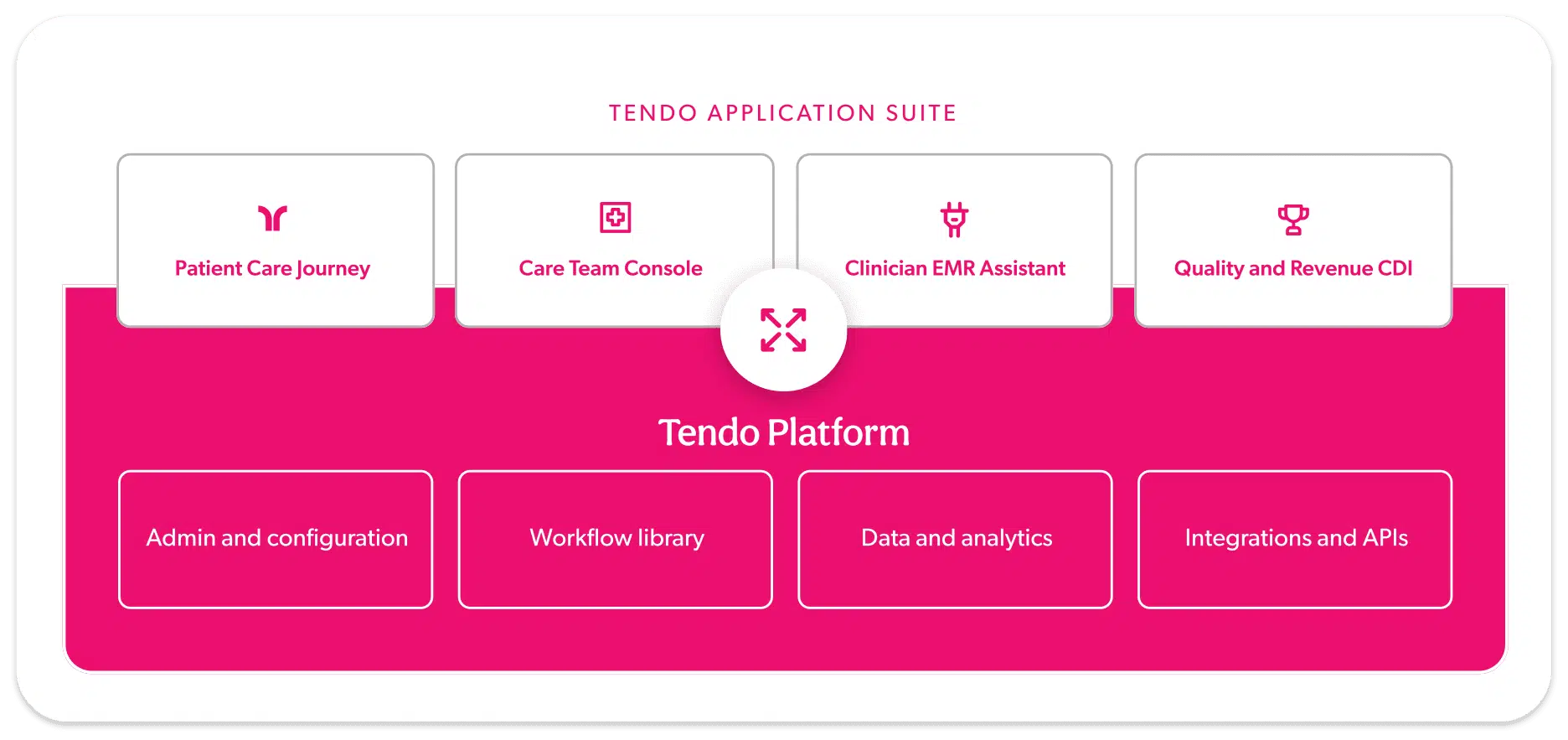
I’ve joined Tendo because this holistic vision is in the DNA, and we have put in the hard upfront R&D work to create the best foundation in the industry. Coupled with a strategic co-design model with our health system partners, we feel strongly about engineering efficiency for staff and intuitive journeys for patients to scale personalized care. Tendo—an unmatched leading platform for the future of care delivery.
learn more about how we can help.
Tendo can give you the building blocks for your health system’s digital transformation.